Cornea Transplant
A Closer Look at Cornea Transplants
Do I Need Surgery?
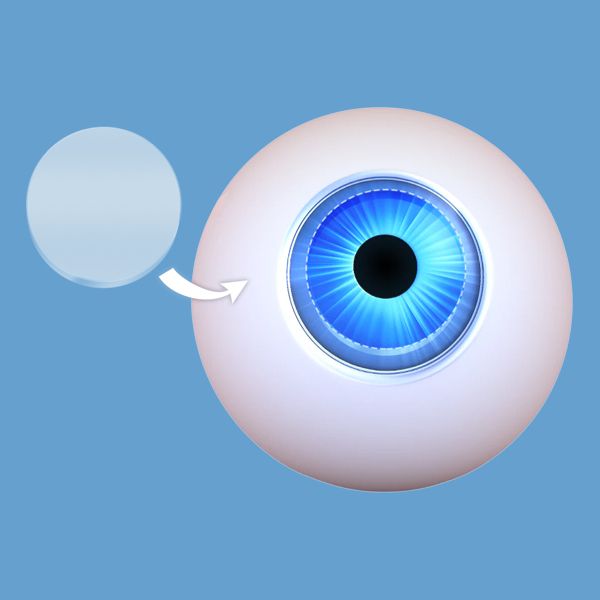
The cornea is the clear layer at the front of the eye. Injuries or diseases such as corneal dystrophy or keratoconus can leave the cornea scarred or opaque and distort your view of the world. If the cornea cannot be healed or repaired and your eyesight cannot be corrected using eyeglasses, contact lenses, or refractive surgery, our ophthalmologist in Dallas, TX, can perform a cornea transplant using a donor cornea.

What Can Surgery Achieve?
Our highly qualified surgeons use the latest proven corneal transplant techniques, such as DSEK (or DSAEK) and DMEK (or DMAEK). These advanced measures allow us to tailor surgery to patients' needs and promote faster recovery and better outcomes.
Corneal transplant surgery can:
• Restore functional vision
• Reduce pain
• Improve the appearance of a damaged cornea

A Surgical Overview
During corneal transplant surgery, a circular piece of the damaged corneal tissue is removed. It is replaced with a “button” of clear healthy cornea donated from an eye bank, which follows federal regulations to ensure only healthy donor tissue is used.
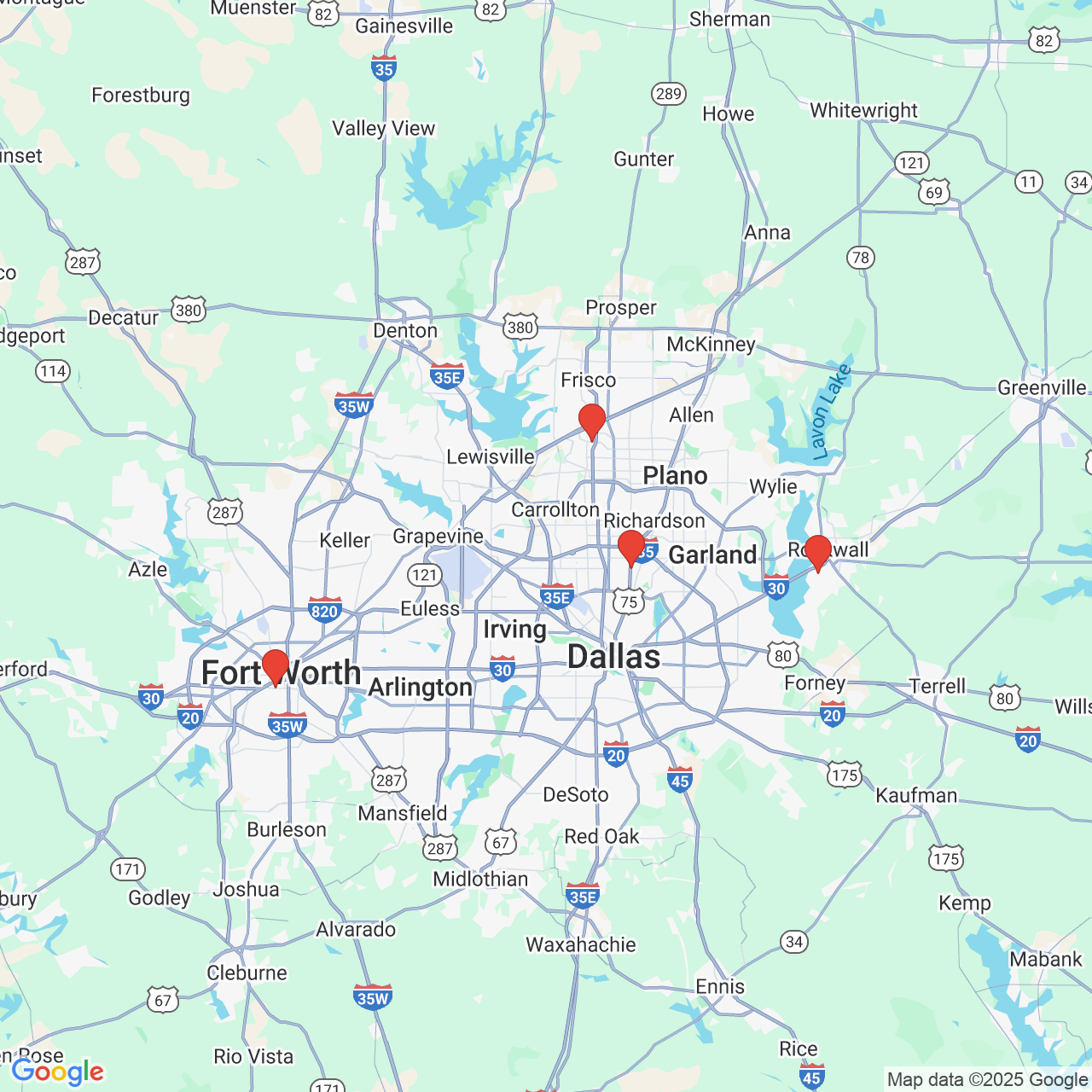
Contact Cornea Associates of Texas In Dallas, Plano, and Fort Worth, TX
The surgeons at Cornea Associates of Texas are recognized by their peers as authorities on refractive errors and corneal problems. If corneal damage or keratoconus is impairing your vision, contact our ophthalmology offices in Dallas, Fort Worth, and Plano, TX.
Expertise and a Personal Touch Our Cornerstones of Care
Our surgeons perform about 900 corneal transplantation procedures each year in a highly selective process. Before recommending this procedure, we carefully evaluate each patient during a personal consultation. We also offer extensive pre- and post-operative counseling so patients understand what to expect at every stage of treatment.
Types of Corneal Transplants
There are several types of corneal transplants. They differ depending on which corneal layers are replaced. Penetrating keratoplasty (PK) involves all layers of the cornea. Newer transplant techniques are limited to individual layers of the cornea.
The surgeons at Cornea Associates of Texas are specifically trained to perform corneal transplant surgery. In addition to being board certified, they have also received advanced cornea fellowship training. They are experts in both traditional and advanced transplant techniques.

Your Comfort Comes First
Your concerns about vision surgery and your comfort are priorities at Cornea Associates of Texas. We have exemplary safety protocols, and our advanced techniques and technology put patients in safe hands.
During transplants, our surgeons use an anesthetic blocking technique that eliminates all sensation and movement from the eye.
The patient is briefly asleep while the anesthetic is administered, then awakens, and surgery is performed with the eye completely numb. The patient is also given IV medication specifically to help them relax and to minimize any anxiety, all while being closely monitored by an anesthetist.
"Would highly recommend" Hear from Cornea Transplant Patients
Dr. Zaffos is an amazing Dr. He actually did my first ever full cornea transplant. And he’s about to do my second. Very nice doctor. He knows what he is doing. I would highly recommend/refer him! This is the place to be if you have eye problems.
View on GoogleDr. Zaffos did a Cornea Transplant on me, and I have subsequently visited his office in Ft. Worth more than a dozen times. I’ve found Dr. Zaffos to be skilled, knowledgeable, personable, positive, and upbeat. He really is just a good guy. If my loved ones needed advanced vision care, I would insist they go to him. The staff there have always been personable, professional, and attentive to concerns. In all my time of going there, I have not had a bad experience. Not one.
View on Google